Written by: Y. Razvi, H. Wong
Medical science has evolved. Unfortunately, the delivery of healthcare itself has changed little over the past 100 years. The COVID-19 pandemic has given us an opportunity to rethink this situation. The widespread adoption of technology and remote care in medicine has already started this transformation from a centralized to a distributed healthcare system.
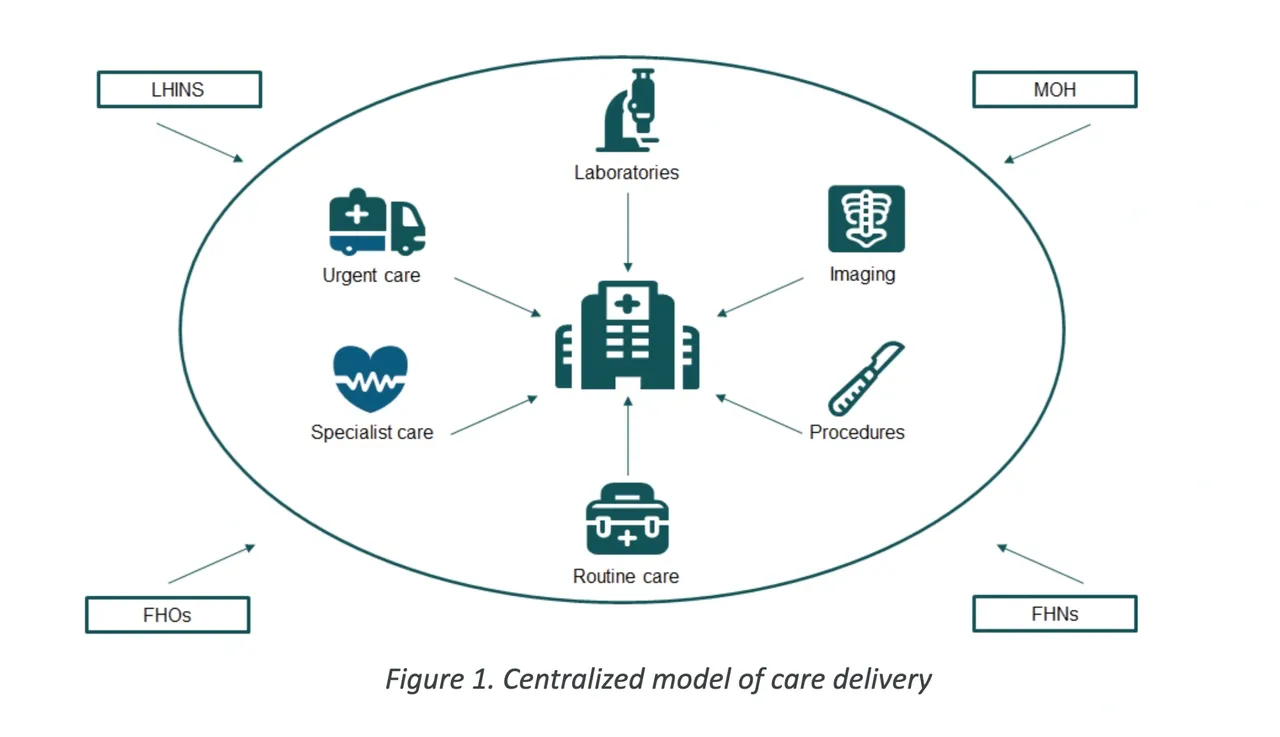
The model of our current healthcare system has developed over the past century. Unfortunately, this means that we have inherited inefficiencies that have created barriers to providing good care. Today’s healthcare system includes both provincial governing bodies such as the Ministry of Health (MOH) and regional entities such as the Local Health Networks (LHINs). At a patient-care level, this system also includes multi-provider Family Health Networks (FHNs) and Family Health Organizations (FHOs). As a result, hospitals play a central role in our healthcare system. FHNs and FHOs refer patients to the emergency departments, medical wards, and surgical suites of their local hospitals. Specialized providers often cluster and seek privileges around local hospitals to gain access to patients and scarce resources such as operating time. Investigations such as routine labs and imaging are also centered around these hospitals. Finally, government entities such as the MOH and LHIN find it convenient to finance and promote healthcare objectives primarily through these hospital networks. In many ways, communities and their local health care systems have been built entirely around their local hospitals, in what we describe as centralized care.
Historically, hospitals were expected to meet all the health-related demands of their communities. This includes universal and equitable access to healthcare resources, access for marginalized and underserved communities, and availability of mental health services. Unfortunately, budgetary, staffing, and capacity restraints often limit the services a hospital may be able to provide. Medical science has also become more complex, making it harder for individual hospitals to provide a complete range of services. As a result, it has become increasingly common for hospitals to reduce their services, either specializing in a few areas or providing a more superficial level of care to a broader group of areas. This creates a situation of unequal access to care across the province. Families that live in smaller, rural communities are forced to travel longer distances to gain access to the same level of care available in large downtown urban centers. This places the burdens and costs of transportation, parking, remote accommodation, and loss of productivity from either work or school on the families themselves.
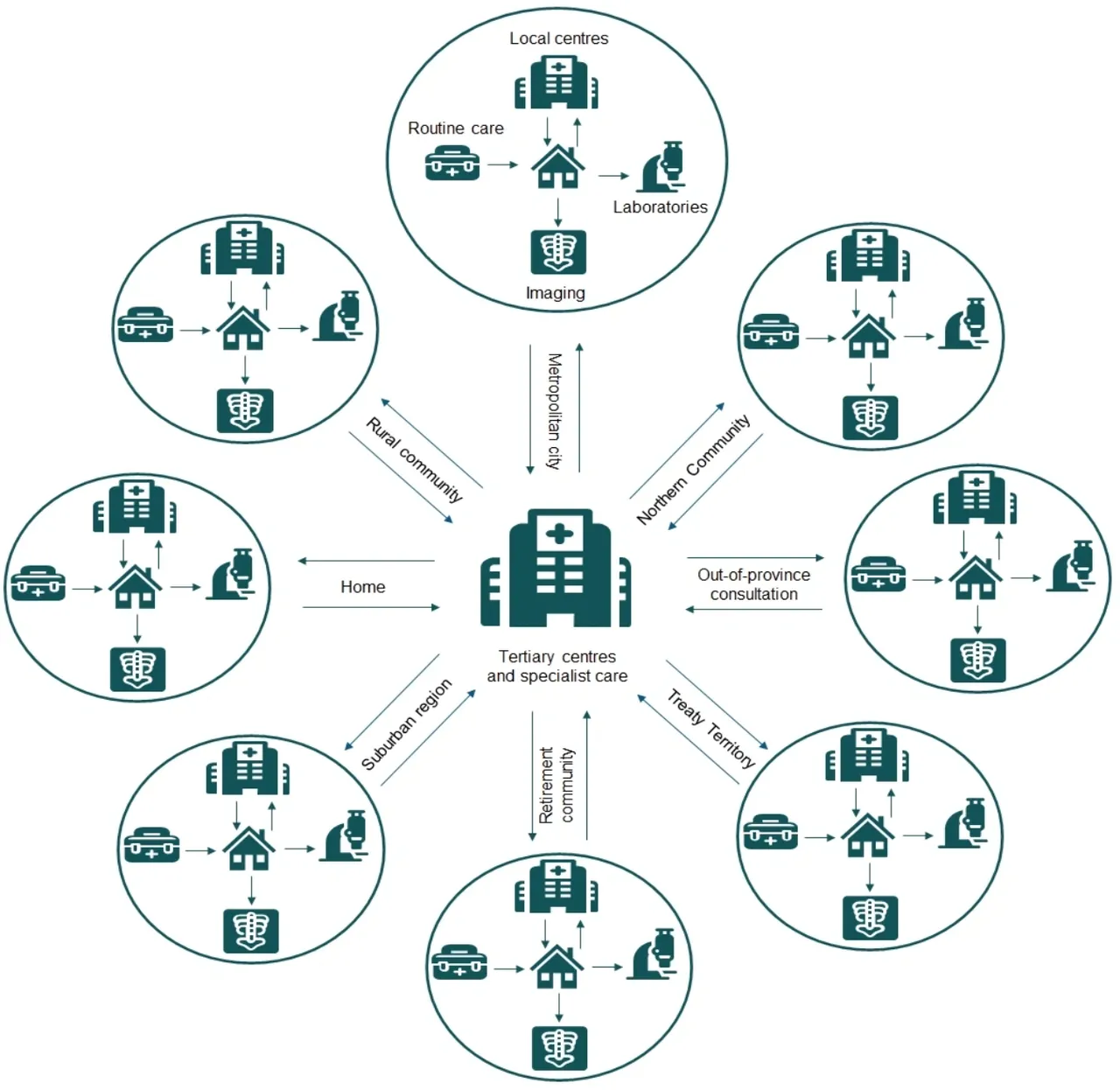
Figure 2. Distributed model of care delivery
The widespread adoption of mobile devices, broadband internet and telemedicine, has provided us an opportunity to change to a more distributed model of care. Medical services do not need to be constrained by the finite resources of a physical building. We can now provide nearly limitless, at-home access to medical services using a combination of remote care, healthcare directed self-assessments, and local diagnostic imaging and testing laboratories. These services are also no longer defined by geographic area. High quality specialized care and counselling that were previously only available in large urban centers can now be easily accessed across the province through virtual or telephone-based communications. This increased access to specialized care in localized areas is what we describe as distributed care.
The pandemic has forced us to rethink medicine. Distributed care is a more accessible, equitable and efficient healthcare system for everyone. Governments should consider this model while they build towards the future.
Resources:
Icons for graphics from https://www.flaticon.com/
